SAN DIEGO – Seventeen of 425 children who had eosinophilic esophagitis caused by a specific food developed the condition after outgrowing the allergy to that food, a retrospective study found.
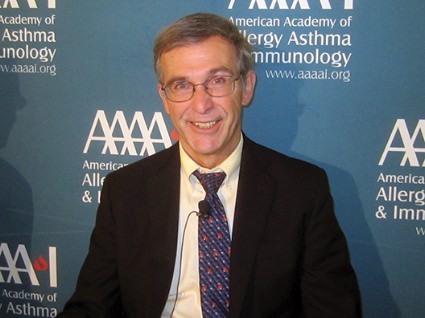
People who outgrow a food allergy may be at risk of developing eosinophilic esophagitis (EoE) to the same food, Dr. Jonathan Spergel said during a press briefing at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
He and his associates studied data on 1,025 children with EoE seen at the Children’s Hospital of Philadelphia in 2000-2012 to assess the prevalence of food allergy. In 425 children (42%), a specific food was identified as the EoE culprit – reintroducing the food to the diet caused esophageal changes on biopsy or biopsy changes normalized when the food was removed from the diet.
Eighty-four children had a history of IgE-mediated food allergy. Milk, egg, wheat, and soy were the most common food triggers of EoE in the 425 children in the study and in a subset of 17 who had outgrown IgE-mediated allergy to the specific food, reported Dr. Spergel, chief of the allergy section at the Children’s Hospital of Philadelphia. Sixteen of the 17 patients had atopic disease. The most common foods causing IgE-mediated allergy were peanuts, tree nuts, eggs, and milk.
The development of EoE coincided with reintroducing the food triggers. The time between outgrowing an allergy and reintroducing the food, triggering EoE, averaged 2 years but ranged from 6 months to 5 years.
Notably, two of the children who outgrew their food allergy had a normal biopsy of the esophagus when they had the food allergy, he said.
The findings support other recent studies suggesting that the pathophysiologies of EoE and IgE-mediated food allergy are distinct from each other, and that both can occur in the same individual to the same food, Dr. Spergel said. The mechanism by which EoE develops is poorly understood.
"I think these kids probably always had EoE to the food, but they weren’t eating it" because of the allergy, he said. "From 1% to 15% on oral immunotherapy get EoE, depending on which group you look at. I don’t think we caused" EoE by giving oral immunotherapy, he added. "We uncovered it."
Although it is rare for children who outgrow a food allergy to later develop EoE to that food, it’s worth keeping in mind if a child starts vomiting often or complains of stomachaches months or years later, Dr. Spergel said. Keeping the possibility in mind may help clinicians rule out other etiologies and detect EoE faster. "You have to take it seriously and get it checked out," he said.
Of the 84 patients with IgE-mediated food allergy, the 17 who outgrew the allergy and then developed EoE to the same food were significantly older (12 years, on average), compared with 67 patients who developed EoE from a different food from the one that caused their allergy.
The lead author on the study was Dr. Solrun Melkorka Meggadottir, a fellow at the Children’s Hospital of Philadelphia. The findings have been submitted to the Journal of Allergy and Clinical Immunology.
Dr. Spergel and Dr. Meggadottir reported having no relevant financial disclosures.
On Twitter @sherryboschert