WASHINGTON – A third more Americans were hospitalized for ischemic stroke in 2010 than 7 years before, and the incidence of stroke associated with atrial fibrillation grew even more sharply, up by 42% in 2010 relative to the 2003 rate, according to nationwide data collected in the Nationwide Inpatient Sample.
The period 2003-2010 also witnessed other notable changes in hospitalized U.S. patients with stroke or atrial fibrillation (AF) or both. The in-hospital mortality rate of hospitalized stroke patients with AF dropped from 12% in 2003 to 9% in 2010. During the same period the prevalence of hospitalized AF patients with a high stroke risk, identified by a CHADS (congestive heart failure, hypertension, age > 75 years, diabetes, and prior stroke or transient ischemic attack) score greater than two rose from 20% of hospitalized AF patients in 2003 to 29% in 2010, reflecting an increased prevalence of the comorbidities that drive the CHADS score. The prevalence of a prior stroke or transient ischemic attack (TIA) among hospitalized American AF patients jumped from 5% in 2003 to 12% in 2010, Dr. Arun R.M. Sridhar said at the annual meeting of the American College of Cardiology.
In a multivariate analysis, prior stroke or TIA was the strongest risk predictor for a subsequent stroke among the hospitalized AF cases in the data base, said Dr. Sridhar, a physician at the University of Kansas Medical Center in Kansas City.
But increases in the prevalence of prior stroke and TIA as well as in other measured comorbidities and the growing elderly population with AF and stroke were together unable to fully explain the rising rate of AF-associated strokes. "The rise in strokes persists despite accounting for the changes in demographics. The reasons are not very clear," Dr. Sridhar said.
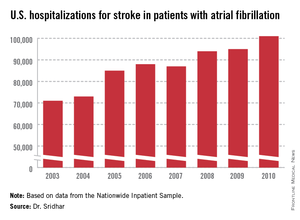
The Nationwide Inpatient Sample data, collected annually by the Agency for Healthcare Research and Quality, showed that total U.S. hospitalizations for stroke rose from about 335,000 in 2003 to 448,000 in 2010, a 34% jump over 8 years. During the same time stroke hospitalizations for patients with AF increased from about 71,000 in 2003 to 101,000 in 2010, a 42% relative spike. This means the percent of hospitalized stroke patients who also had AF inched up from 21.2% in 2003 to 22.5% in 2010.
One of the clear drivers of the increase in AF-associated strokes was an aging population. In 2003, 37% of AF associated, hospitalized strokes were in patients aged 85 or older. By 2010, the 85 and older segment had swelled to 42%. The statistics also showed discernable but slower growth in patients aged 65-84 years, as well as in women and whites.
Mortality among hospitalized stroke patients fell across the board, not just among those with coexistent AF. For hospitalized stroke patients without AF in-hospital mortality fell from 5.1% in 2003 to 4.1% in 2010. During the 8 years, the average length of hospitalization dropped by about a day for all stroke patients, but despite that inflation-adjusted hospitalization charges jumped by 27% for patients with stroke and AF and by 39% for those with stroke and no AF.
Dr. Sridhar and his associates also analyzed data from more than 27 million Americans hospitalized with AF during the 8-year period. During this time the prevalence of several comorbidities in AF patients all rose and drove up their CHADS scores, starting with the increased prevalence of a history of stroke or TIA. The prevalence of hypertension in hospitalized AF patients rose from 45% to 48%, the prevalence of concomitant heart failure rose from 31% to 37%, and the prevalence of diabetes rose from 24% to 29%. But all these increases, as well as older patient ages, could not fully account for the 42% jump in the total of hospitalized stroke patients with AF from 2003 to 2010, Dr. Sridhar said.
Dr. Sridhar and his associates said that they had no disclosures.
On Twitter @mitchelzoler