A hospital’s rate of postoperative Clostridium difficile infection is related to the number of preoperative antibiotics patients have taken, the complexity of their procedures, and the complexity of the hospital’s surgical program, in addition to known risk factors for the infection, according to a report published online in JAMA Surgery.
Several risk factors for postoperative C. difficile infection have already been identified, including advanced age and comorbidity. To examine known risk factors and identify possible new ones, researchers analyzed information from the Veterans Affairs Surgical Quality Improvement Program’s database, which documents all noncardiac operations at 134 VA medical centers each year.
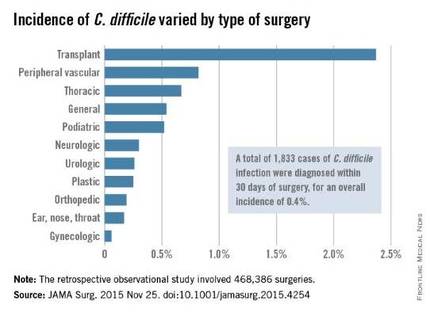
The investigators focused on 468,386 procedures performed during a 4-year period. A total of 1,833 cases of C. difficile infection were diagnosed within 30 days of surgery, for an overall incidence of 0.4% in this predominantly male, elderly population, said Xinli Li, Ph.D., of the Veterans Health Administration, Washington, and associates.
As expected, patients who developed postoperative C. difficile infection were significantly older than those who didn’t (mean age, 67.4 vs. 60.6 years) and were significantly more likely to have comorbidities such as impaired functional status, heart failure, chronic obstructive pulmonary disease, ascites, renal failure, bleeding disorders, wound infection, and recent weight loss.
Unexpectedly, the number of different antibiotics taken during the 60 days preceding surgery also was significantly associated with C. difficile infection. Patients who had taken three or more antibiotics from different classes were nearly six times more likely to develop C. difficile than patients who had taken only one or no antibiotics, the investigators reported (JAMA Surg. 2015 Nov 25. doi: 10.1001/jamasurg.2015.4263).In addition, patients who underwent more complex surgical procedures were at increased risk of this complication, as were patients at hospitals that frequently handled complex procedures. “These factors reflect the illness of patients, duration of operation, and hospital setting; each is an established risk factor for C. difficile infection,” Dr. Li and associates wrote.
Patients with C. difficile infection had higher rates of postoperative other morbidity (86.0% vs. 7.1%) and 30-day mortality (5.3% vs. 1.0%) and longer postoperative hospital stays (17.9 days vs. 3.6 days).
Contrary to previous studies, this study did not show a temporal increase in C. difficile infection. The overall incidence, as well as the incidences at individual hospitals, remained constant during the entire 4-year study period, the investigators added.
The incidence of C. difficile varied substantially among the 134 VA medical centers, from 0% to 1.35% of all surgical patients. “Surgical administrators and clinical teams may consider the results of this study to target interventions for specific patients undergoing high-risk procedures. Such interventions include selective antibiotic administration, early testing of at-risk patients, hand hygiene with nonalcohol agents, early contact precautions, and specific environmental cleaning protocols,” Dr. Li and associates wrote.
This study was supported by the Veterans Health Administration. Dr. Li and associates reported having no relevant financial disclosures.